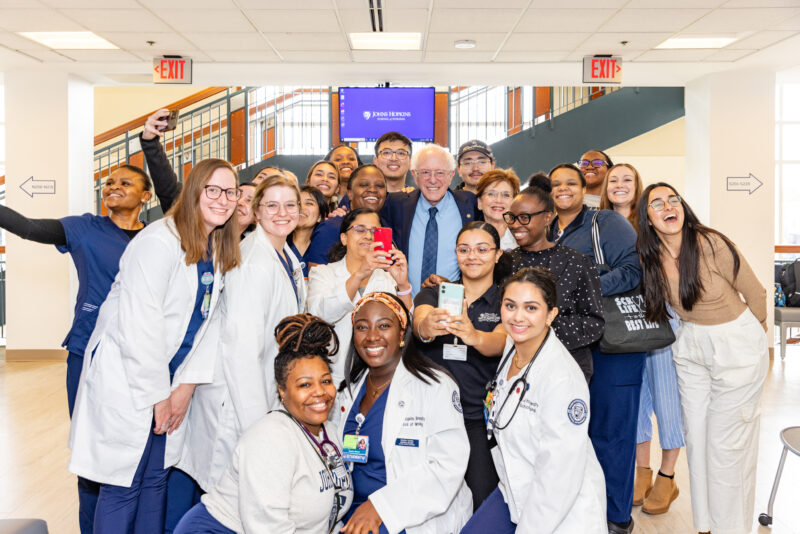
In April 2017, Johns Hopkins School of Nursing (JHSON) students attended the Consortium of Universities for Global Health Conference, “Healthy People, Healthy Ecosytems,” in Washington, D.C. Students wrote blogs reflecting on breakout sessions and topics presented by experts and the current climate of global health. In part seven, we look at the thoughts of JHSON student Hyejeong Hong and and non-communicable diseases in low- and middle-income countries.
“Beyond epidemiology of injuries, turning evidence into policy and practice!”, Adnan A. Hyder, Associate Chair, International Health, Johns Hopkins Bloomberg School of Public Health, USA
Dr. Hyder evoked the meaning of injury in the context of global health. I didn’t realize that there is a intersection of global health and injury! I had a dichotomized definition of global health issues, for example, communicable vs. non-communicable diseases. He classified “injury” as any type of injuries threatening one’s health or well-being, such as traffic accidents, falling accidents, homicide, and sexual violence by extending their definitions to a macro level of injury. Dr. Hyder insisted that turning scientific evidence into policy and practice is challenging. He stressed that “we have to be free from zero sum game” in the context of global health. He said that many experts emphasize “my disease is X million dollars and your disease is Y million dollars…” for public acknowledgement, however, several conditions that are hard to measure, like injuries, are often neglected because injury prevention takes a particularly long time to realize benefits. It will require explicit attention, new skills, and investment to achieve the impact from injury prevention. He gave me a chance to think and shift the paradigm of global health problems from diseases to injuries. For example: car safety seats are mandatory in the US and other developed countries but we don’t use the equitable rule in LMICs. We may need to map out our life threats in the same manner.
“What makes young people more vulnerable to NDCs?”, Moffat Nyirenda, Professor of Global Health, London School of Hygiene and Tropical Medicine, UK.
Before attending this conference, I believed that obesity is associated with affluence and that obesity is an independent and concrete risk factor of NCDs including hypertension or diabetes. In contrast, Dr. Nyirenda presented a very interesting argument where “phenotype risk factors of NCDs differ from genotype factors.” In his analysis, Nyirenda found that “low birth weight would be a significant surrogate marker of increased risk of hypertension or diabetes.” From several retrospective cohort studies, hypertensive and/or diabetic patients living in sub-Saharan Africa typically had a history of low birth weight. His hypothesis on this phenomenon was that premature babies may have low energy for sufficient physical activities, leading to increased risk of high blood pressure and/or insulin resistance and when they stop growing, their adipose tissues tend to save surplus energy easily. Thus, they become obese although they consume very minimal calories. Currently, many global health programs or projects use diuretics as a first line medication for hypertension and metformin for diabetes under the assumption that the leading cause is obesity, as is the case in developed countries. However, this is not true in sub-Saharan Africa, and we should not overlook the possibility of pancreas or kidney damage from first line medications, which will make recipients dehydrated and worsens health outcomes. We, as health care providers, should seriously consider the uniqueness of individuals to bring about the optimal health outcome.
“Leveraging the infectious disease platform in the health system to provide chronic care of NCDs”, Kaushik L. Ramaiya, CEO, Shree Hindu Mandal Hospital, Tanzania.
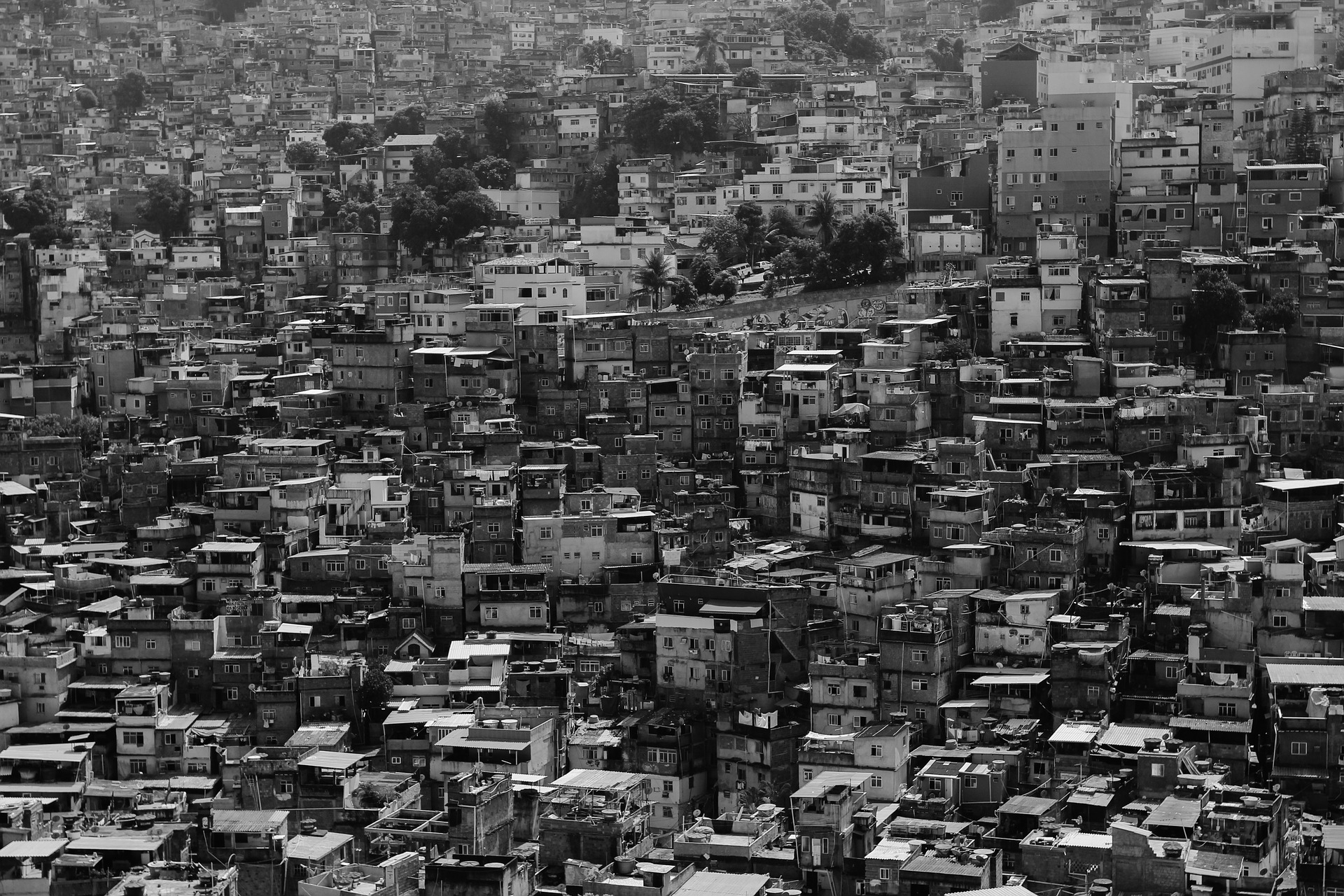
Constructing health care infrastructure is one of the challenges for global health programs. Many LMICs have fairly organized communicable disease care facilities, for example community-based tuberculosis or HIV clinics and centralized referral systems when a communicable disease is suspected or confirmed. He suggested, “community-based primary care services can be utilized for general screening or individual health education about hypertension and diabetes.” If patients need more intensive care, then health care providers, including doctors and nurses, can refer them to disease-specific services. Community health workers still provide education, screening, and treatment adherence while regional or district level services prescribe medications periodically with clinical and laboratory evaluations. Through his talk, I realized that there is no need to separate communicable and non-communicable disease facilities if appropriate isolation is guaranteed. This platform sharing strategy can not only be cost-effective but also clinically effective by monitoring within an accessible distance.